Published by The Commonwealth Institute.
1. Rural hospitals would face a rising tide of uninsured patients who are unable to pay for care. The American Health Care Act (AHCA) – the recently passed House bill – would increase the number of low- and moderate-income Virginians without adequate health coverage, pushing the costs of care onto hospitals. That’s because it would slash Medicaid funding, something that will hit particularly hard in rural areas of Virginia where people are nearly twice as likely to be on Medicaid as in other areas of the state. Combined with cuts in the supports that make health insurance more affordable for older moderate-income people, the number of Virginians without adequate health insurance would increase sharply. Nonprofit rural hospitals would increasingly be on the hook to pick up the costs because when patients are unable to pay, hospitals usually have to absorb more than half of the cost of care, something that’s known as uncompensated care cost (UCC).
Prior to the Affordable Care Act (ACA), rural hospitals across the country were responsible for covering nearly $4 billion annually in UCC. The AHCA is estimated to swell this amount to $7 billion in just the first year alone. On average, nearly 7 percent of hospitals’ costs are already attributed to UCC, and given the fragile profit margins of Virginia’s rural hospitals, increasing this share further could spell disaster for those on the brink. Hospitals act as essential safety-nets for those in rural communities without coverage, but these institutions can only sustain so long when operating at a loss and providing an increasing amount of UCC.
2. Rural hospitals are already struggling to stay open and the AHCA will make it more likely they will be forced to close. In 2015, nearly half of Virginia’s rural hospitals had negative operating margins. The AHCA’s planned cuts to Medicaid and the subsequent increase in the number of uninsured Virginians who rely on uncompensated care will just make this worse. Under the assumption that all states would expand Medicaid, Disproportionate Share Hospital payments (DSH), a program to offset the costs of providing care to patients who don’t have insurance and can’t afford to pay for care, is scheduled to begin decreasing this upcoming year. DSH has been an important lifeline for rural hospitals, which often treat more low-income patients who are less likely to have coverage and be able to pay for their care. The AHCA does not reverse the downward path for DSH payments until 2020, and if AHCA passes, rural hospitals will be receiving less compensation for treating those unable to pay precisely at the moment when more of their patients are losing coverage.
3. The AHCA removes a critical tool that Virginia could use now to help stabilize rural hospitals. Medicaid expansion was meant to be the safeguard for rural hospitals, ensuring that a larger share of their patients had health coverage, and the hospitals weren’t left to pick up the check for as many uninsured patients as DSH payments declined. Rural hospitals in Medicaid expansion states have seen their profits grow more than urban hospitals. Passage of the AHCA now would lock Virginia out of this expansion option, which most other states have already taken advantage of, and would put Virginia on track for even more rural hospital closures in the future.
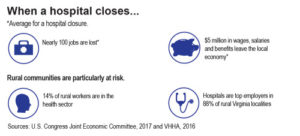
4. Hospitals are bedrocks in rural economies, often serving as the largest employer and source of health services in a given area — meaning that the impact of closure as a result of the AHCA would be devastating to many of these communities. In 2015, hospitals were the top employers in 88 percent of rural Virginia localities. When hospitals close, there is an economic harm associated with the disappearance of a significant share of an area’s good-paying jobs, and adverse effects on community health outcomes due to reduced care options. Virginia’s Lee Regional Medical Center in rural Lee County is one example of the hardship facing rural hospitals. The facility closed its doors in 2013, resulting in the loss of nearly 140 good-paying jobs in the local community. (Negotiations are underway to try to re-open that facility, but meanwhile residents are without a hospital.)
5. Rural hospitals serve as a lifeline for rural communities, and more closures would lead to a decline in the health of rural residents. Families and individuals in rural communities throughout the state are more likely to be covered by Medicaid, have additional health issues, be lower-income, and have to travel further for care than urban communities. We know that when individuals have to travel further for hospital care, their health outcomes tend to decline and mortality rates increase. Closure of rural hospitals or a reduction in coverage may cause individuals such as seniors to forego regular preventive care, and instead lead to more uncompensated emergency care and deteriorating health conditions. The AHCA would both threaten the solvency of rural hospitals and reduce the level of coverage in rural communities, thereby contributing to a perilous scenario for rural communities and their hospitals.
–Chad Stewart, Research Assistant




